What Is the Medical Billing Process? Steps & Cycle Overview

Accounts Receivable (A/R) follow-up ensures outstanding balances are collected efficiently. Encourage patient engagement through clear explanations of their financial responsibilities upfront. This proactive approach reduces confusion and follow-up inquiries related to bills. Therefore, diligent follow-up is necessary if there are issues or outstanding balances. Once the claim has been created, coded, http://mozitamigration.co.nz/simplified-payroll-for-the-way-your-ministry-works/ and scrubbed, it is submitted to the insurance company for reimbursement.
Phase 1: Pre-Visit Medical Billing Workflow
But this step-by-step guide will make things through for you or any new billers interested in the industry. Alongside your patient statements, you should send payment instructions and due dates. You can also include information on how the patient can appeal the claim denial if they feel so inclined. Often, medical practices or their Outsource Invoicing outsourced billing teams manage denials, but the patient may still want to file appeals on their own. Instead, if you see that your claim is denied because the insurer doesn’t cover your services, you have two options.
Step 7: Payer Adjudication
- To overcome the challenges in claim submission, healthcare providers should adopt a combination of technology, training, and streamlined workflows.
- Alternatively, you can outsource your medical billing services to a trusted provider like Nexus io.
- You can also include information on how the patient can appeal the claim denial if they feel so inclined.
- Machine learning algorithms can adapt over time, improving accuracy with each transaction.
- In some cases, a claim may only appear to be a duplicate, such as when a patient receives the same service from a different practice on the same date.
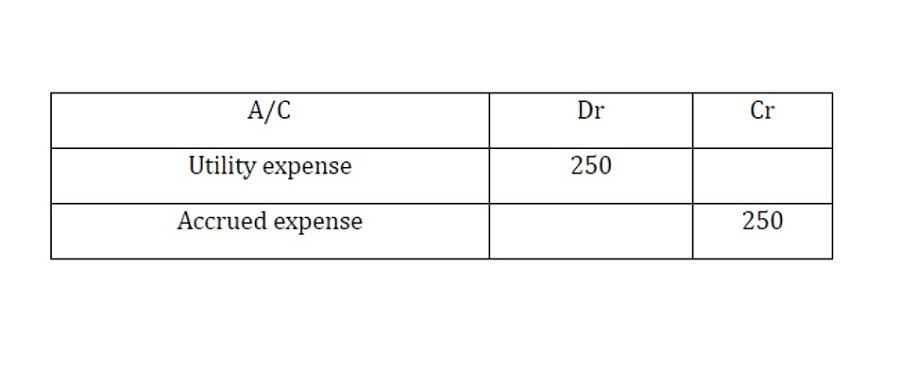
Make life easier on yourself and your staff by using the future of medical billing software to improve your revenue cycle management. Payment posting is the step where payments made by insurance providers, patients, third parties, or any government programs (like Medicare and Medicaid) are recorded in the billing system. It involves the process of correctly identifying received payments, aligning them with the patient accounts, and updating the financial records accordingly.
Claim Submission Workflow

Transforming your healthcare facility’s revenue cycle starts with choosing the right medical billing process steps medical billing partner. MDS brings decades of expertise in streamlining the medical billing process, helping practices reduce administrative burdens while maximizing reimbursement rates. The right software will make patient registration easier with electronic forms and automated data entry.
- This claim is then «scrubbed,» a term for a final audit to catch errors before it is sent to the payer.
- This article explains the 12 core medical billing process steps, offering a clear framework for healthcare providers, office administrators, and billing specialists.
- Denial management is most effective when handled by an experienced medical billing team or uses AI-powered tools to automate tracking, prioritization, appeals, and prevention workflows.
- By examining each stage, from initial patient contact to final account reconciliation, you can identify areas for improvement and ensure a more predictable revenue cycle.
- From the front desk to the back office, focusing on accuracy and efficiency at each stage will reduce errors, improve cash flow, and lead to a better financial experience for patients.
If you’ve voice-recorded any of your notes without using voice-to-text tools, you’ll need to transcribe them before sending them to your medical billing team. Chances are you won’t have the time to do this yourself, so you might delegate the work to your front office staff. Alternatively, you can outsource this work to a medical transcription service.


Dejar un comentario
¿Quieres unirte a la conversación?Siéntete libre de contribuir